My source of inspiration
It is amazing (and sometimes scary) what can go through our minds during a solitary drive. While taking a solo road trip through beautiful southern Utah, I starting thinking about cars. I guess it makes sense seeing that I had been in one for hours as I was approaching Bryce Canyon National Park. I felt a lot of appreciation for some of the safety features that I did not have on my previous cars like the rearview camera, proximity sensors for merging, and bluetooth to safely handle incoming phone calls. I was in awe over how much the automobile has really evolved.
There were already a variety of different steam and gasoline powered cars that had been invented before Henry Ford came along to introduce the fairly affordable Model T in 1908. Those initial Model T’s had no wheel brakes, optional windshield wipers, no radio, all while having a max speed of 45 mph. I’m guessing it was a heck of an upgrade from getting around on horses.
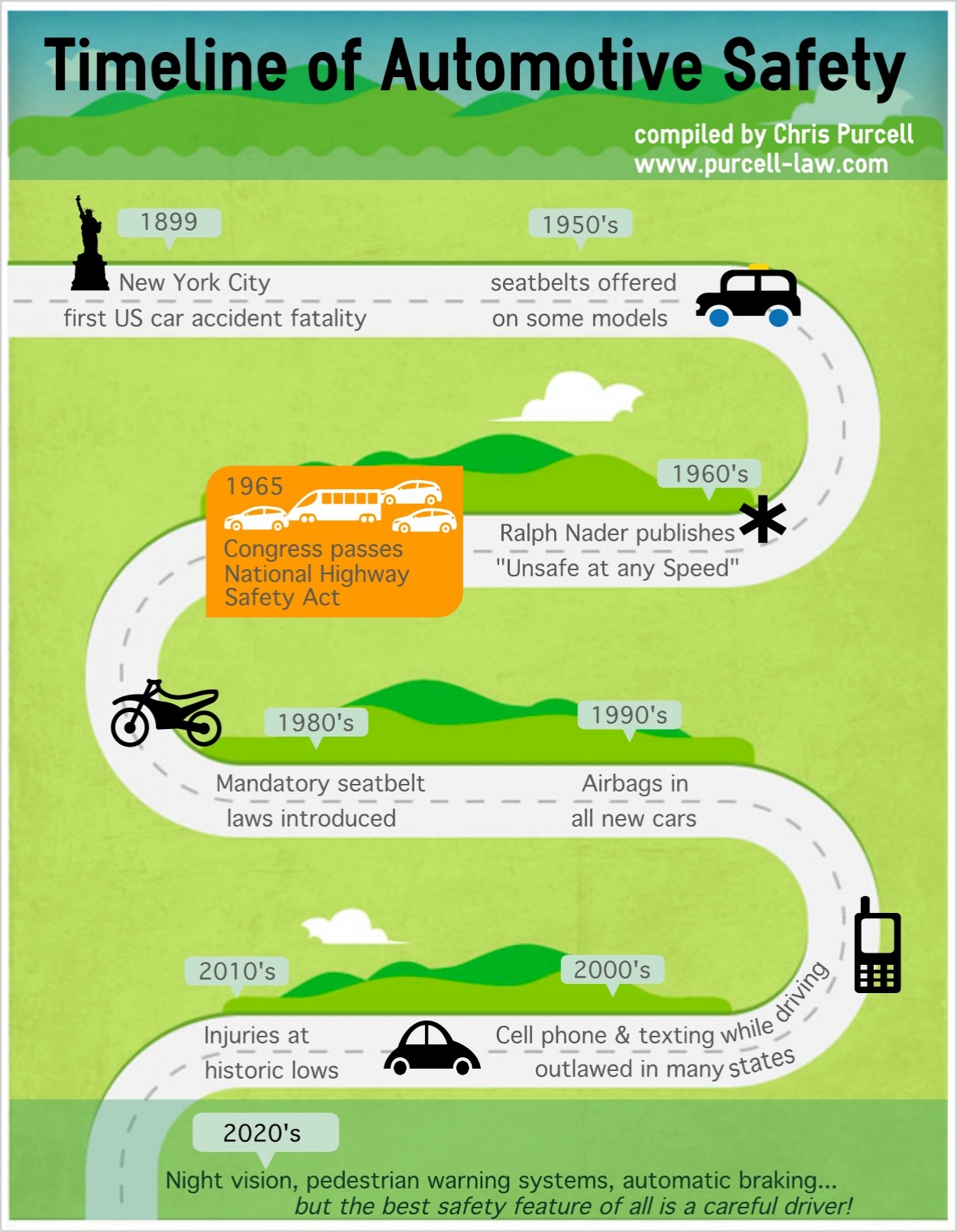
From a safety perspective, the evolution of the automobile was fairly slow: seat belts were not a standard feature in any car until Saab did it in 1958. Not that it mattered much since it took nearly another 30 years for them to be required by law in the United States. The progression has seemed to move faster since the first airbags were added in the 1990s. Now we have those cameras and proximity sensors. Human error may be removed completely in the near future since we may not have to even manually drive cars.
That is not to say driving a car is still a perfectly safe endeavor. Accidents still happen. Console designs can still use a little work. One of my friends recently shared her story of a near accident while she was changing the internal temperature. Instead of a knob, the control was a button that required more of her attention which was not on that other car on the road. After over 100 years of evolution that has given us some amazing achievements, safe driving technology still has not been perfected.
This mini-revelation got me thinking about healthcare IT, patient safety, and User Experience. On their own, each of these fields are still relatively new:
- EMR giant, Epic, was founded in 1979.
- The first book on usability that I ever read was Jakob’s Nielsen’s “Usability Engineering”, which was first released in 1993. Don Norman’s “The Design of Everyday Things” was published 7 years earlier.
- The infamous "To Err is Human: Building a Safer Health System” report that launched numerous patient safety research initiatives just turned 15 last year.
- And the stimulus package that created the Meaningful Use initiative and boosted the Health IT world was passed in 2008. Which is around the same time I first heard the term “user experience”.
I have been working in the unique crossroads of Health IT, Patient Safety, and UX for over 10 years. It has certainly been a chaotic ride. I have often wondered how many more stories from clinicians about the poor usability of their software that I can stomach to hear. How much longer can I continue to beat my head against the wall as I see designs cut down due to technical and business constraints. How much more finger pointing between clinicians, hospitals, and vendors will continue on as the patients have little say on the situation.
The reality is: These are still young fields, and I have been living in their adolescent phases. Of course it is chaotic. Of course there are complaints about HIT usability. Of course the culture change that has to follow rapid technology advances feels like it is moving like a glacier. If 100 years of automobile evolution hasn’t made driving a perfectly safe endeavor, how is it possible we have made Health IT perfectly safe and usable in 20-30 years?
Looking at the big picture, amazing steps have been taken in these last 10 years. I am so much more efficient at wireframe design and recording usability tasks because of the tools now available to me. There are companies with Chief Experience Officers. There are many new organizations that are focused on patient safety initiatives and health IT improvements. The occurrence of ICU blood stream infections has decreased. Good user-centered design practices are no longer a nice to have in healthcare, but have become a competitive necessity. If you like to follow the money - over $4 billion was invested in digital health start ups last year! And frankly, my Twitter feed is overwhelming most days when I look at the amount of information that is available to me in just seconds.
I guess if I took anything away from my road trip, it’s that I need to not be so frustrated that the junction of health IT, UX, and patient safety are not in this ideal place where I want it to be. We have come a long way, but there is a lot more work to be done. All of us - clinicians, health systems, vendors, designers, developers, etc - have to work together to evolve our fields in the right direction. Just the fact that the AMA is asking the ONC to change EHR certification to focus on “usability, interoperability, and safety” shows me that we are indeed continuing to evolve. So let’s roll up our sleeves, stop pointing fingers, focus on the patients that need our help, and go build great healthcare products!
I am really excited to see where this evolution will bring us in ten years…